
Physician Assistant (PA) Program
At A Glance
Accreditation
Visit our accreditation page for details
Format
In person, full time, curriculum infused with problem-based learning
Location
Newberg, Oregon
Application Deadlines
End of April to September 1 (rolling admissions)
Cost
PANCE & Goal Attainment Info
Visit our mission page for details

Care for One. Care for All.
You’ll promote the well-being of every patient you serve as a PA, but we don’t want you to stop there. We’ll put you in a position to transform entire communities.
At George Fox, you’ll develop innovative treatment plans with your peers, put your knowledge to work in an array of clinical settings and extend compassion to high-need areas across the globe. You’ll learn how to bridge the gap where medical services are scarce – and the care you provide as a physician assistant/associate will resonate across generations.
Nurture a Healthy Future
Drive innovation in one of the nation’s top facilities, fast-track your doctorate (DMSc) degree and emerge as a leader in patient-centered care.
-
Compassionate & Collaborative
Join a close-knit learning community of 36 students who share a passion for expanding access to essential health care and services.
-
Energized by Technology
Our Medical Sciences Building features patient exam rooms, 3D Anatomage Tables, group study spaces that facilitate problem-based learning and dedicated areas for focused research.
-
Elevated by Expertise
Forge lasting relationships with expert educators and practitioners who connect you with personalized learning opportunities and professional networks that span the globe.
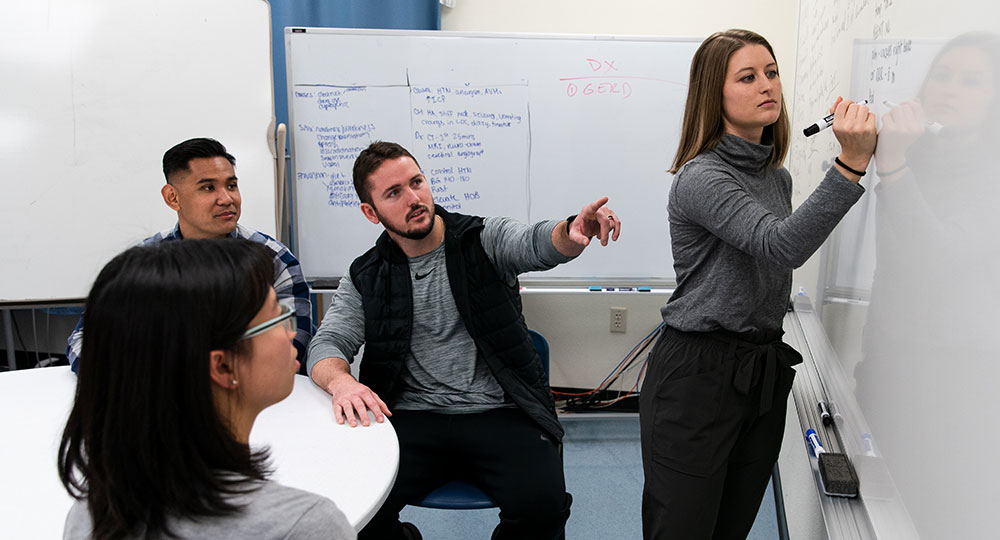
Tackle Complex Cases
Collaborate with your peers in small groups to address the medical issues of actual patients. It’s all part of problem-based learning, a teaching approach that emphasizes developing new knowledge instead of memorizing the right answer. You’ll hone your analytical skills and learn to convey complex information with precision and clarity.

“It’s a different kind of experience,” says 2023 graduate Sarah Jane Lance, who’s re-establishing orthopedic care as a PA in Harney County, Oregon. “You’re working not only alongside your classmates but with them, which reflects what you’ll be doing as a practitioner. Being pushed to be in these groups and work through things together is challenging, but it forces you to grow.”

Serve from the Heart
We’ve created a culture of leadership, knowledge and humanitarian service in our learning community with a special focus on rural and medically underserved communities. Our vision is to transform the medical field by increasing access to high-quality, affordable care. This is your chance to bring health and healing to those who need it most.

“With the knowledge that I gained through school, I have the kuleana – the responsibility – to go back home someday and take care of the people of my community,” says 2023 graduate Tia Kinilau. “If you take care of the community, it will take care of you.”
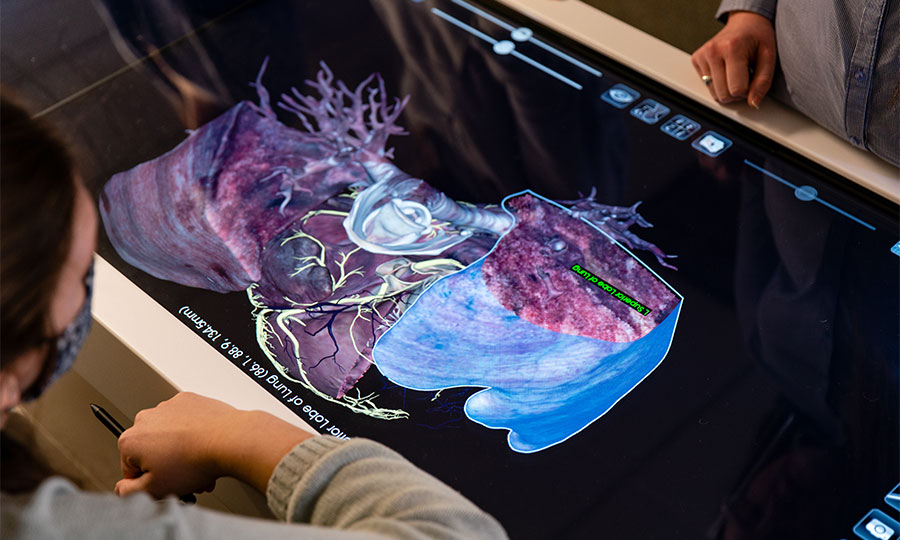
Learn on the Leading Edge
Master the latest technology in our 43,000-square-foot Medical Sciences Building. You’ll gain insights from practicing PAs in state-of-the-art classrooms, hone your skills using cutting-edge tools and create knowledge through research. We share the building with our physical therapy program, opening the door to collaborative projects and insights that transform your life’s work.

“The PA program aligns directly with my dreams, goals and passions while allowing me the opportunity to provide quality and affordable care,” says Christina Cranley, a PA specializing in primary care in Roseburg, Oregon. “I truly couldn’t see myself attending anywhere else.”

Accelerate Your Career
Thanks to our dual-enrollment format, you can start working toward your doctorate (DMSc) degree right away. You’ll complete 21 DMSc credits during your first two years in the PA program, giving you the option of earning your Doctor of Medical Science degree with one additional semester of three online classes. You’ll also gain invaluable experience during a weeklong service trip to a high-need community domestically or abroad.

“The DMSc degree sets the graduate up to be a leader in disaster medicine relief and health care delivery to communities in high need,” says Curt Stilp, associate dean of the College of Medical Science and director of the PA program. “It brings the mission of humanitarianism and service to fulfillment through advanced knowledge, research and experience.”

Be Close to Everything
George Fox University is located in the beautiful Pacific Northwest, home to lush green valleys, breathtaking vineyards, windswept beaches, and mountains that extend from the Coast Range in the west to the high desert in the east.
Newberg, home to George Fox, is situated along the Willamette River between the Oregon Coast and the spectacular Cascade Mountains. Whatever your interest, it’s probably just a short drive away.
- 45 minutes to the vibrant cultural life of Portland
- 60 minutes to the Pacific Ocean
- 90 minutes to the slopes of Mt. Hood
State Licensure Links & Reciprocity Table
Students earning their license through the George Fox PA program have reciprocity to practice in all 50 U.S. states.
| State | Does student have reciprocity to practice in the state? | Link to State Licensing Agency for Inquiries re: New License | ||
|---|---|---|---|---|
| Yes | No | Don't Know | ||
| Alabama | Yes | AL: PA Licensing | ||
| Alaska | Yes | AK: PA Licensing | ||
| Arizona | Yes | AZ: PA Licensing | ||
| Arkansas | Yes | AR: PA Licensing | ||
| California | Yes | CA: PA Licensing | ||
| Colorado | Yes | CO: PA Licensing | ||
| Connecticut | Yes | CT: PA Licensing | ||
| Delaware | Yes | DE: PA Licensing | ||
| Florida | Yes | FL: PA Licensing | ||
| Georgia | Yes | GA: PA Licensing | ||
| Hawaii | Yes | HI: PA Licensing | ||
| Idaho | Yes | ID: PA Licensing | ||
| Illinois | Yes | IL: PA Licensing | ||
| Indiana | Yes | IN: PA Licensing | ||
| Iowa | Yes | IA: PA Licensing | ||
| Kansas | Yes | KS: PA Licensing | ||
| Kentucky | Yes | KY: PA Licensing | ||
| Louisiana | Yes | LA: PA Licensing | ||
| Maine | Yes | ME: PA Licensing | ||
| Maryland | Yes | MD: PA Licensing | ||
| Massachusetts | Yes | MA: PA Licensing | ||
| Michigan | Yes | MI: PA Licensing | ||
| Minnesota | Yes | MN: PA Licensing | ||
| Mississippi | Yes | MS: PA Licensing | ||
| Missouri | Yes | MO: PA Licensing | ||
| Montana | Yes | MT: PA Licensing | ||
| Nebraska | Yes | NE: PA Licensing | ||
| Nevada | Yes | NV: PA Licensing | ||
| New Hampshire | Yes | NH: PA Licensing | ||
| New Jersey | Yes | NJ: PA Licensing | ||
| New Mexico | Yes | NM: PA Licensing | ||
| New York | Yes | NY: PA Licensing | ||
| North Carolina | Yes | NC: PA Licensing | ||
| North Dakota | Yes | ND: PA Licensing | ||
| Ohio | Yes | OH: PA Licensing | ||
| Oklahoma | Yes | OK: PA Licensing | ||
| Oregon | Yes | OR: PA Licensing | ||
| Pennsylvania | Yes | PA: PA Licensing | ||
| Rhode Island | Yes | RI: PA Licensing | ||
| South Carolina | Yes | SC: PA Licensing | ||
| South Dakota | Yes | SD: PA Licensing | ||
| Tennessee | Yes | TN: PA Licensing | ||
| Texas | Yes | TX: PA Licensing | ||
| Utah | Yes | UT: PA Licensing | ||
| Vermont | Yes | VT: PA Licensing | ||
| Virginia | Yes | VA: PA Licensing | ||
| Washington | Yes | WA: PA Licensing | ||
| West Virginia | Yes | WV: PA Licensing | ||
| Wisconsin | Yes | WI: PA Licensing | ||
| Wyoming | Yes | WY: PA Licensing | ||
Questions?

Tabitha Hall
Admissions Counselor, PA Program